Introduction to What Does Patient-Centered Care Mean?
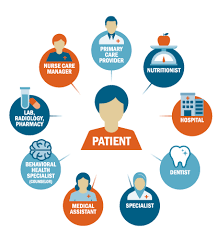
Even though the healthcare system has improved in several ways over a long period, one thing that is quite striking is the idea of What Does Patient-Centered Care Mean?. It is correct; it is patient-centered care, but over the years, does this even mean anything? Patient-centered care is a method that looks forward to addressing the patient’s wants and the treatment process from the beginning. This is no longer just a fad; this is a change in the economics and mechanics of the healthcare business.
What if you entered a healthcare facility where you were listened to, your past was considered, and your feelings were at the driver’s seat in deciding the health offered? This is not as unrealistic as it appears; these developments are becoming achievable as many providers` systems architecture is organizationally adapted to this. As will be seen, patient-centered care is not an isolated approach that hails from history. Some rules define it, and the healthcare industry strives to gain something from it in every sense and form. Stand with us and explain why patients’ first approach should provide some critical understanding of health and wellness design.
Table of Contents
The History and Evolution of Patient-Centered Care
The notion of putting the patient first has always existed. As earlier mentioned, the management of human health was centered on illnesses and not patients, which led to many patients believing that they were mere puppets.
This changed in the 1960s as dignity became a central issue in patient care. Debates began on the need to address the patient’s wishes.
Over the next few decades, an emerging academia suggested that if people understood the patient’s journey, their results would improve. As the 20th century progressed, “patient-oriented care” expanded within the medical milieu.
In the late 1990s, Associations such as the Institute of Medicine described its importance in enhancing healthcare delivery systems. These days, it’s regarded as a basic procedure in several health systems across the globe, complementing treatment with clinical skills for total healing.
The Key Principles of Patient-Centered Care
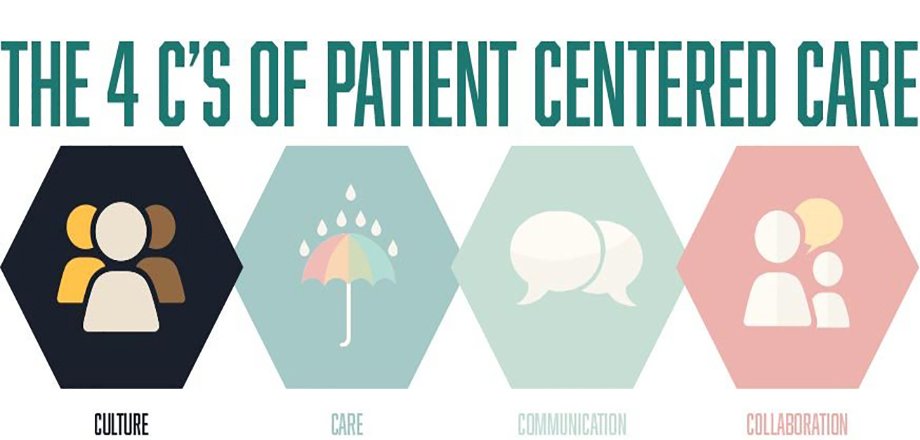
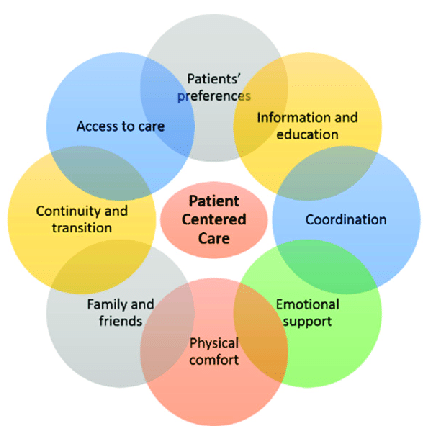
Informed consent is regarded as a key ethical principle in CMI, and this practice goes hand in hand with the principle of patient-centered care. Since every patient is different, patients cannot be treated in this manner; therefore, such treatment options should be based on the patient.
Partnership and cooperation are yet another role player. They help develop a continuum among clients and healthcare providers. Lifted communication barriers facilitate the free exchange of information, which is vital for understanding baby care practices.
Accessibility plays a vital role as well. Patients need to easily access services, resources, and support systems that are tailored to meet their corresponding needs.
Care continuity issues are out of the question. There are no hitches in how patients progress from one stage of treatment to another, making them feel at ease in their journey.
Patients are moving towards taking charge of their own health by embracing empowerment. Highly educated individuals are in a position to choose issues that concern them.
Heuristic approaches seem to treat a patient’s physical condition, feelings, and social circumstances as well. Such an approach covers every aspect of health care.
Benefits of Implementing Patient-Centered Care
These include operational efficiencies realized in health systems, such as patient-centered care. Firstly, it improves patient-provider interactions. People will be more cooperative and adhere to their treatment plans when they know they have been listened to.
Another merit that deserves a mention is increased satisfaction. Patients express higher satisfaction levels when their care is centered on their interests and needs.
Moreover, this is also likely to result in improved health status. More targeted strategies usually adhere better to treatment plans based on the patients’ reasoned choices.
Cost-effectiveness is also a consideration. Such healthcare systems will help reduce unnecessary hospital admissions and emergency visits by focusing on prevention and health education programs.
Trust is cultivated in this culture because it is directed at the patients. Conversely, this trust enhances relationships and encourages patients to express their health concerns openly. This scenario also benefits everyone involved in delivering or receiving health care services.
Challenges to Achieving Patient-Centered Care
Patient-centered care is achievable but only with several challenges. One such challenge includes barriers such as communication and language. Regarding health literacy among patients, it is often hard for many of them to take an active role in their care.
Another issue is the need for more integration among health systems. When there are isolated healthcare providers, the patient may have a problem with care continuity. This lack of integration can create conflicts in a given treatment regimen and even become a challenge for the patient.
Still, the need for more resources is a big hurdle. Many healthcare facilities cannot operate due to having few staff members and their budget limiting the time set for each patient.
In addition, cultural variations may be a barrier to effective relations between patients and their providers. It has to be emphasized that sufficient training and experience must be imparted for them to handle such distinct cultures.
Some institutional barriers to the nightmare include adherence to patients’ preferences and change progress barriers to patients toward implementing patient-centered care practices. It requires consistency and a change in gears faster than organizational levels can manage.
Examples of Successful Implementation in Healthcare Settings
Various healthcare institutions have accepted PCH with good results. Cleveland Clinic stands apart for its deliberate effort to use patient-centric feedback mechanisms. In this respect, they open interaction channels and help the patients be heard and appreciated.
Another one is the organization Planetree, which also provides healing to patients. They attempt to include artistic creations in the structure of the hospitals, as well as natural elements and spaces for the community. This promotes patient healing, and it is additionally ideal for patience to blossom in such an atmosphere.
A third example is the Group Health Cooperative in Washington State. They set up collaborative health decision-making tools that enable patients to participate in the decision-making about what procedures they undergo. Because of this partnership, patients’ satisfaction rates and health results have increased.
Cockcroft et al. transformed the health care services as they attained the middle ground by supporting the patients and engaging them afterward. Challenges notwithstanding, that case remains a stalemate and a nuisance towards quality and efficient health care delivery.
How Can Patients and Providers Work Together for More Effective Patient-Centered Care?
The focus on the patient’s healthcare or treatment becomes a joint effort because patients have caregivers caring for their treatment. Why any type of relationship is essential will be apparent at some point in the partnership. Further, patients should have no reason to hide from their health providers any matter, including any problems, wishes, or even their preferences.
To gain the patient’s trust, the practitioners may either listen to their concerns and comments or inquire, arousing their trust through any other action. This is possible even with the most difficult patients. A common vision of treatment objectives and the scope of good communicative interactions between the participants are formed because of the good communicative interactions they know about them and the treatment they are offered; the more active they become in all the stages of care. Negative shows can be polished by using more positive concepts to call patients to participate.
Technology can also facilitate interdependence and teamwork. Telehealth offers an opportunity to help students throughout the process while allowing them to express their worries or questions about their health at that moment.
Conclusion: The Importance of Prioritizing Patient Needs in Healthcare Systems
Enhancing healthcare systems by eliminating barriers to accessing and receiving care is fundamental to building a sense of worth and importance in everyone. Subsequently, when Embracing Care services from health providers that embody the needs of health services as perceived by the patient, focusing on those aspects patients consider important enhances relations, hence health status.
Patients and healthcare providers work hand in hand. However, the latter is the dominant figure in this relationship, ensuring that healthcare delivery is holistic and more satisfactory. Healthy relations enhance communication, on the other hand, to enhance patient treatment, where various considerations need to be made on the treatment plans. This alone not only helps the individual clients but also benefits the entire structure of health services.
With What Does Patient-Centered Care Mean becoming increasingly prominent, it becomes evident that acquiring its principles can result in improved interactions within the clinical environment. When patient preferences are placed at the forefront, there is always a benefit, both in terms of patients and within the medical practices themselves—higher patient satisfaction rates and improved efficiency.
The commitment to these findings guarantees that both parties are driven towards even better health outcomes. Underlining this principle will catalyze a better tomorrow where every patient’s care and choices are considered in health care matters.
FAQs
What Does Patient-Centered Care Mean?
Patient-centered care is a common style of healthcare that emphasizes patients’ needs and respects their ‘ignoring,’ as they are cornered in it. This means that patients are also involved in the process rather than just passive recipients, and the focus is more on the individual and interaction as well as treatment.
What are the major advantages of a patient-centered care strategy Compared to conventional practices? What are The methods of health care delivery?
Patient-centered care also considers a patient’s dignity and individuality, considering their strengths, emotional requirements, and journey through the illness. Contrary to typical models that are mostly dependent on conformance and paperwork, the focus is on people, how they feel, and what they need to do to improve.
Why Is The Care Of Patients Inclusive In Such A Way That It Is Done Outside Of The Hospitals Where They Get Their Treatments?
Patients in the centre of care bear the outcomes with satisfaction, impart the required health and social needs, and encourage reasonable conversations between patients and care providers. Whenever care is offered to the patients and their needs, even their emotions, are accentuated, organizations provide optimum care to their patients.
What Are The Effective Features Of The Patient-Centered Care Model Of Care?
Key principles include obtention of informed consent, partnership and cooperation, access ability, continuity of care, fostering independence, endorsement, and a broad approach to meeting biological, psychological, and sociological purposes.
What Are The Issues Relating to The Practice of Patient-Centered Care?
Issues include communication barriers, lack of health system integration, inadequate resources, and cultural and organizational barriers. Resolving these problems is a long-term process that requires the appropriate effort from doctors and patients.
What Are The Success Stories Of Patient-Centric Care In Health Facilities?
They include using Zocdoc to enhance patients’ clinical outreach initiatives at the Cleveland Clinic, incorporating healing settings into hospitals designed by Plane tree, and the decision-making processes employed by Group Health Cooperative. The former illustrates various ways of providing care by emphasizing patients.
Why Is Patient-Centered Care Effective For Health Outcomes?
Patient-centered care embraces the active participation of the patient in their care and takes care of the unique needs and wishes of the patient, which translates to greater compliance with treatment menus, greater satisfaction, and improved health results.
To what extent are Arise Benefit Plan clients looking to use technology to provide patient-centered care acquisition?
Technological advancements, such as the use of electronic records, telehealth, patient portals, and other tools, enhance patient-centered healthcare practices by improving communication, making information available, and consequently creating more tailored plans for patients.
As the needed reforms and change cannot be achieved overnight, what strategies can Healthcare systems implement?
Healthcare systems can assist this evolution by expanding coverage, providing provider training, adopting practices that put the patient at the centre, improving care accessibility, and creating an environment that supports and values the patient’s needs and choices.

